IADR Abstract Archives
Standard- versus low-dose CBCT in decision-making for impacted third molars
Objectives: To investigate whether there were significant differences in the diagnostic variables and treatment decisions for impacted mandibular third molars (M3M) between paired standard- and low-dose cone-beam computed tomography (CBCT) as evaluated by dental practitioners with different qualifications.
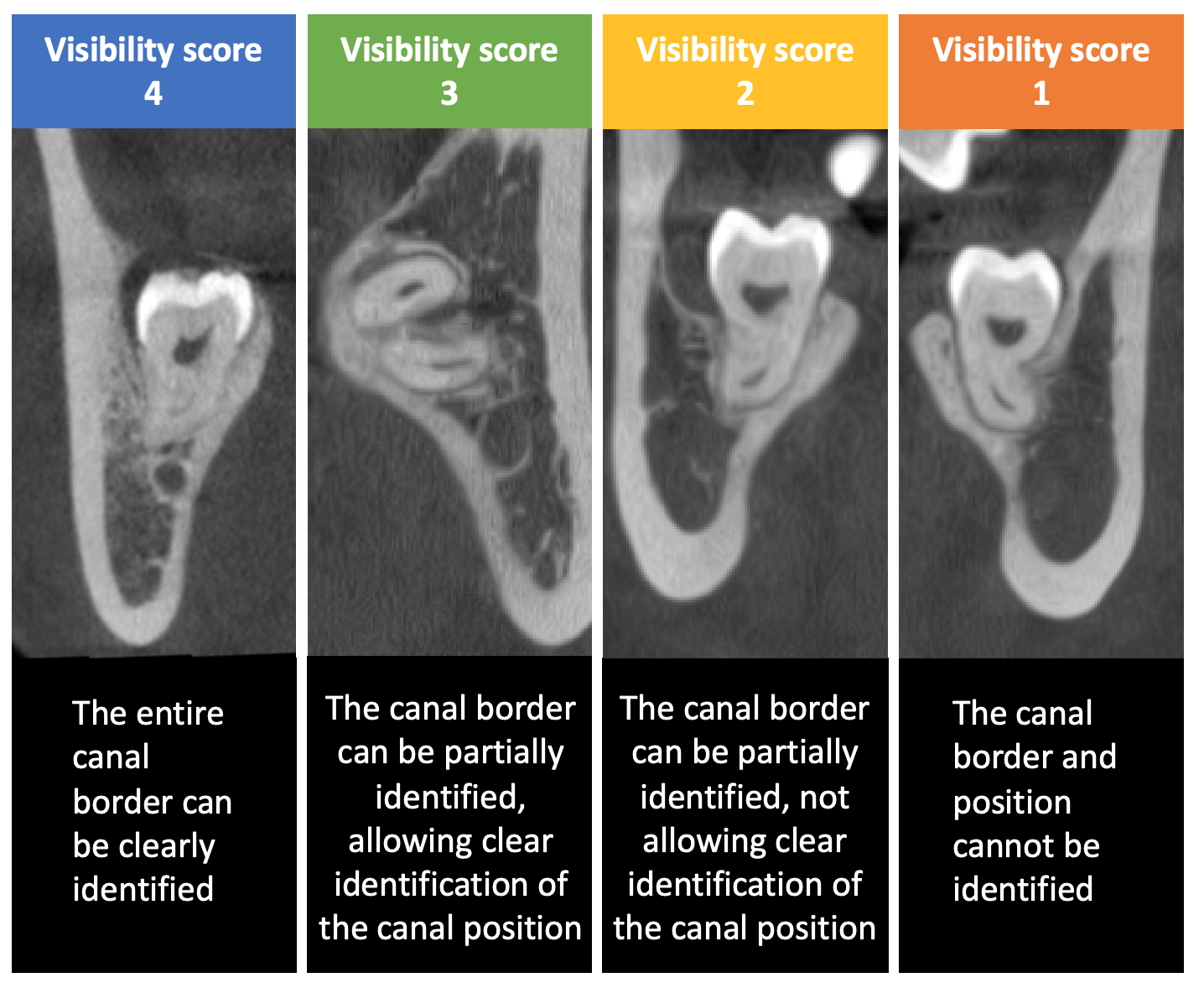
Methods: A randomised non-inferiority clinical study was conducted involving patients with an impacted M3M indicated for removal and panoramic radiograph showing ≤2mm between the mandibular canal (MC) and an M3M. The patients’ M3Ms were randomly assigned to three groups for two small field-of-view CBCT scans performed using one standard-dose (333mGy×cm2) and one of the three low-dose (78-131mGy×cm2) protocols, with doses equivalent to panoramic radiography. Diagnostic variables (MC visibility on four-point scale and the risk of inferior alveolar nerve injury) and treatment decisions (surgical approach between full removal and coronectomy, referral to an oral-maxillofacial surgeon (OMFS), and the need for M3M crown/root sectioning) were assessed on both paired low- and standard-dose CBCT images by four blinded general practitioners and OMFSs. The differences in all variables between paired low- and standard-dose CBCTs were evaluated using Wilcoxon signed-ranks or McNemar test.
Results: A total of 154 paired CBCTs were obtained from 90 patients. Standard-dose CBCTs were deemed diagnostically acceptable in 85-99% of cases, with a visibility score of ≥3 across four observers. Inferior MC visibility was found in 2-31% of low-dose CBCTs compared to paired standard-dose images. No significant differences were found in all treatment decisions regarding surgical approach (p=0.453-1.000), referral (p=0.250-1.000), the need for crown (p=0.125-1.000)/root (p=0.07-1.000) sectioning between paired standard- and low-dose CBCTs for all three groups.
Conclusions: The three low-dose CBCT protocols were clinically acceptable for M3M management without significant changes in treatment decisions, regardless of the observer’s qualification, when compared to paired standard-dose scans. The implementation of low-dose CBCT protocols, with doses equivalent to panoramic radiography, would not significantly affect clinical decision-making in M3M management.
Methods: A randomised non-inferiority clinical study was conducted involving patients with an impacted M3M indicated for removal and panoramic radiograph showing ≤2mm between the mandibular canal (MC) and an M3M. The patients’ M3Ms were randomly assigned to three groups for two small field-of-view CBCT scans performed using one standard-dose (333mGy×cm2) and one of the three low-dose (78-131mGy×cm2) protocols, with doses equivalent to panoramic radiography. Diagnostic variables (MC visibility on four-point scale and the risk of inferior alveolar nerve injury) and treatment decisions (surgical approach between full removal and coronectomy, referral to an oral-maxillofacial surgeon (OMFS), and the need for M3M crown/root sectioning) were assessed on both paired low- and standard-dose CBCT images by four blinded general practitioners and OMFSs. The differences in all variables between paired low- and standard-dose CBCTs were evaluated using Wilcoxon signed-ranks or McNemar test.
Results: A total of 154 paired CBCTs were obtained from 90 patients. Standard-dose CBCTs were deemed diagnostically acceptable in 85-99% of cases, with a visibility score of ≥3 across four observers. Inferior MC visibility was found in 2-31% of low-dose CBCTs compared to paired standard-dose images. No significant differences were found in all treatment decisions regarding surgical approach (p=0.453-1.000), referral (p=0.250-1.000), the need for crown (p=0.125-1.000)/root (p=0.07-1.000) sectioning between paired standard- and low-dose CBCTs for all three groups.
Conclusions: The three low-dose CBCT protocols were clinically acceptable for M3M management without significant changes in treatment decisions, regardless of the observer’s qualification, when compared to paired standard-dose scans. The implementation of low-dose CBCT protocols, with doses equivalent to panoramic radiography, would not significantly affect clinical decision-making in M3M management.