IADR Abstract Archives
Periodontal Treatment on Patient With Hematologic Disorder: A Systematic Review
Objectives: To determine the periodontal management of a patient with a hematologic disorder
Methods:
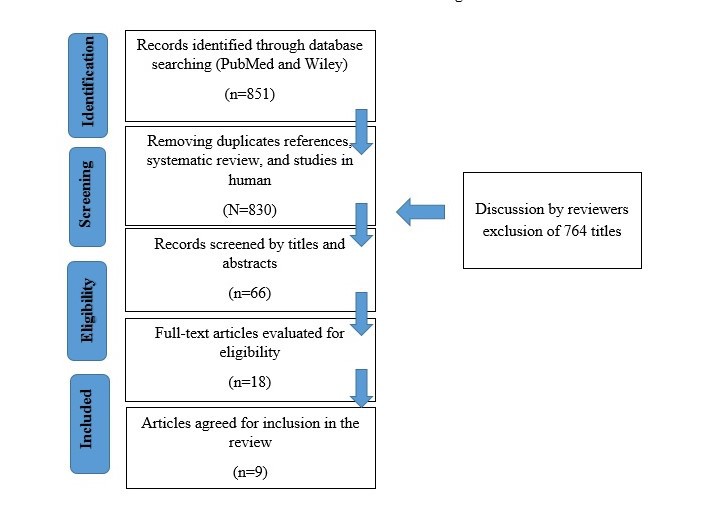
Electronic Pubmed and Wiley searches were conducted to identify articles published in dental journals from April 2008 to April 2018 focusing on periodontal treatment in the hematologic patient. Manual searches of published full-text articles and related reviews were performed afterward. There are 18 studies explained about this with 9 studies met the inclusion criteria
Results: The initial database search produced 851 titles. All articles were selected for full-text review. 9 studies were selected for inclusion, with 12 patients as subjects. Most of the periodontal treatment were nonsurgical therapy with systemic medication. A detailed knowledge of intra-operative and postoperative measures of the patient is considered a priority for the dental care professional
Conclusions: The management of a hematologic patient with periodontal disease requires a multidisciplinary comprehensive care between hematologist and periodontist. By maintaining the periodontal health, it may prevent the risk of spontaneous bleeding
Methods:
Electronic Pubmed and Wiley searches were conducted to identify articles published in dental journals from April 2008 to April 2018 focusing on periodontal treatment in the hematologic patient. Manual searches of published full-text articles and related reviews were performed afterward. There are 18 studies explained about this with 9 studies met the inclusion criteria
Results: The initial database search produced 851 titles. All articles were selected for full-text review. 9 studies were selected for inclusion, with 12 patients as subjects. Most of the periodontal treatment were nonsurgical therapy with systemic medication. A detailed knowledge of intra-operative and postoperative measures of the patient is considered a priority for the dental care professional
Conclusions: The management of a hematologic patient with periodontal disease requires a multidisciplinary comprehensive care between hematologist and periodontist. By maintaining the periodontal health, it may prevent the risk of spontaneous bleeding
South East Asia Division Meeting
2018 South East Asia Division Meeting (Da Nang, Vietnam)
Da Nang, Vietnam
2018
0090
Periodontal Research - Diagnosis/Epidemiology
Medikawaty, Rahma
( University of Hasanuddin
, Makassar
, Indonesia
)
Thahir, Hasanuddin
( University of Hasanuddin
, Makassar
, Indonesia
)
Mapanggara, Surijana
( University of Hasanuddin
, Makassar
, Indonesia
)
Djais, Arni
( University of Hasanuddin
, Makassar
, South of Sulawesi
, Indonesia
)
Utami, Sari
( UNIVERSITY OF HASANUDDIN
, MAKASSAR
, SULAWEI SELATAN
, Indonesia
)
Madjid, Fatmawati
( university of hasanuddin
, MAKASSAR
, SOUTH SULAWESI
, Indonesia
)
none
2018 South East Asia Division Meeting (Da Nang, Vietnam)
Da Nang, Vietnam
2018
0090
Periodontal Research - Diagnosis/Epidemiology
Poster Session
Poster Session 2-Behavioral Science and Health Services
Thursday, 09/13/2018 , 11:15AM - 12:30PM
Poster Session 2-Behavioral Science and Health Services
Thursday, 09/13/2018 , 11:15AM - 12:30PM
Periodontal treatment on hematologic patient
| No | Author / Year | Number of patient | Age (y.o) | Hematologic disease | Intraoral examination | Periodontal treatment |
| 1 | Soga et al /2008 | 1 | 61 | Acute myeloid leukemia (AML) | The radiographic and gingival appearance showed an advanced chronic periodontitis, loss of 1/3–1/2 adjacent supporting bone with probing depth range from 4-6 mm among almost all teeth | Scaling root and planning was performed in each interval period of chemotherapy followed by periodontal pocket curettage before hematopoietic transplantation (HCT) |
| 2 | Agnihotri et al / 2009 | 1 | 51 | Aplastic anemia | Swelling of the gingiva with spontaneous bleeding after 6 months of cyclosporine therapy, deep pocket (7mm) with pus and grade III furcation involvement on teeth 13 and 25. Panoramic radiograph showed generalized horizontal bone loss | The pockets were irrigated with 0.2% chlorhexidine gluconate and resorbable fibers containing 2 mg of tetracycline were placed in the gingival pocket of teeth 13 and 25. Ultrasoft toothbrush and 0.2% chlorhexidine mouth rinse were used for plaque control. After her platelet count increased to 60,000/μl and neutrophils count increased to 4,600/μl a thorough full-mouth subgingival scaling and root planing were carried out |
| 3 | Guzeldemir / 2009 | 1 | 11 | Idiopathic thrombocytopenic purpura | Gingival inflammation and spontaneous gingival bleeding, abundant supra and subgingival plaque deposits | When thrombocyte count was 144.00 K/mm3 and scaling and root planning of upper and lower anterior region was performed under local anaesthesia, regular dental brushing with a soft-bristle toothbrush and 0.2% chlorhexidine digluconate oral rinse |
| 4 | Nickles et al / 2010 | 4 | 32-60 | Von Willebrand type I and mild hemophilia B | The clinical and radiographic findings yielded a diagnosis of generalized aggressive periodontitis in patient 1, generalized severe chronic periodontitis in patients 2 and 4, and generalized moderate localized severe chronic periodontitis in patient 3 | On the day of SRP, a blood count, global coagulation, and VW tests were performed in each patient. Under local anesthesia subgingival scaling and additiion of an 1% chlorhexidine gel. After SRP, an aqueous solution of tranexamic acid was applied as a mouthwash for 2 minutes in all patients. The patients were instructed to rinse with a 0.12% chlorhexidine solution twice daily and brush their teeth with a 1% chlorhexidine gel |
| 5 | Fang lu and Xin meng / 2012 | 1 | 6 | Cyclic Neutropenia | Gingival recession and teeth mobility, recurrent oral ulcers, and deep caries | After general status of the patient improved and acute gingival inflammation reduced, the patient received nonsurgical periodontal treatment including oral hygiene instruction, 0.12% chlorhexidine gluconate oral rinse, scaling and root planning with no prophylactic antibiotic |
| 6 | Gadagi and Chava / 2012 | 1 | 29 | Congenital afibrinogenemia | No signs of hemorrhage with OHIS 0.9, probing pocket depth measuring >10 mm with mesial 11 and distal 12 was associated with pathological mesiolabial migration and grade II mobility | Initial treatment included Phase I periodontal therapy with systemic medication (amoxicillin 500 mg t.i.d., metronidazole 400 mg b.i.d., diclofenac potassium 50 mg b.i.d. for 5 days), chlorhexidine mouthwash and oral hygiene instructions local drug delivery with chlorhexidine chip was carried out at interval 3-, 6-, and 9-month |
| 7 | Gonzalez and Frydman / 2014 | 1 | 16 | Kostmann syndrome | Gingival inflammation with generalized bleeding on probing (BOP). The probing depths (PD) and recession ranged from 4-6 mm and 1-3 mm. Class I furcation involvement of six sites. Localized mild horizontal and vertical bone loss on radiographic | Scaling and root planing in four quadrants followed by subgingival irrigation with 10% povidone-iodine solution. Maintenance re-evaluation on 3 and 12 months follow up |
| 8 | Hajishengallis et al / 2016 | 1 | 2 | Autoimmune neutropenia | Inflammation of the anterior maxillary gingiva from primary canine to canine, with erythema, edema, and bleeding upon pressure on both the buccal and palatal sides. For maxillary right central and lateral incisors Probing Depth ranged from 2 to 5 mm, Clinical Attachment Level ranged from 1-3 mm, and bleeding on probing was present. No attachment loss and bleeding on probing was generalized. No oral ulcers or tooth mobility were observed, and radiographic examination showed no significant findings | Nonsurgical treatment by mechanical debridement, oral hygiene with tooth brushing and alcohol-free chlorhexidine applications twice daily. Dental prophylaxis was performed (under antibiotic prophylaxis and Surgical treatment by gingivectomy, oral hygiene instructions were reinforced and chlorhexidine application was reduced to one time daily |
| 9 | Fernandes et al / 2016 | 1 | 5 | Kostmann syndrome | Gingival inflammation that characterized by edema and bleeding upon palpation, as well as the presence of dental calculus, intraosseous periodontal pockets and grade 3 tooth mobility of maxillary and mandibular incisors, and of first primary molars | The teeth with advanced periodonti¬tis were extracted. The remaining teeth received conventional periodontal treat¬ment with complete removal and controls bacterial plaque, oral health education, oral hygiene con¬trol (tooth brushing and flossing), topical application of fluoride varnish (sodium fluoride 2,800 ppm) every 3 months, and prescription of amoxicillin in liquid sus¬pension (250 mg/5 ml) at 20 mg/kg/day in divided doses every 8 hours for 10 days that was initiated 1 day before the intervention. Continuous use of a dentifrice containing chlorhexidine glu¬conate 0.12% and sodium fluoride 0.05% and daily mouthwashes with 0.12% chlo¬rhexidine gluconate were prescribed for three times per day |