IADR Abstract Archives
Dentin-Pulp Complex Regeneration: Towards a Paradigm Shift for Dental Practice
Objectives: The status quo for the replacement of the bulk of defected dentin combined with vital pulp therapeutics (VPT) is based on inert biomaterials. This study provides a novel tissue-engineering-based approach for the structural and functional regeneration of the dentin-pulp complex. Human dentin scaffolds (hFDDSs) were impregnated with calcium phosphate nanoparticles (CaP-NPs) encoding for morphogenetic proteins, with perspectives to be applied in a digital dentistry workflow.
Methods: The hFDDSs were EDTA-treated, freeze-dried, and characterized by X-ray powder diffraction (XRD), confocal laser scanning microscopy (CLSM), and scanning electron microscopy (SEM). The CaP-NPs conjugated with plasmids encoding for Dentin Matrix Protein-1 (pDMP1) or Bone Morphogenetic Protein-2 (pBMP2) were synthesized, characterized, and tested in terms of biocompatibility (MTT assay), cellular uptake, and transfection efficiency [flow cytometry, transmission electron microscopy (TEM) and CLSM] on dental pulp stem cells (DPSCs). The construct of hFDDSs impregnated with NPs (NPs-hFDDSs) was tested for cytotoxicity (live/dead staining), and foreign body reaction in vivo (C57BL mice, N=4). Polarization of cells was evaluated by SEM, while odontogenic differentiation by qPCR.
Results: Based on the biocompatibility vs. transfectability results, nanoparticle concentration of 4-μg-Ca/mL was selected to prepare the NPs-hFDDSs. Biocompatibility of NPs-hFDDSs was similar to the control. In vivo experiments showed no foreign body reaction against the construct. DPSCs differentiated into polarized odontoblast-like cells on NPs-hFDDSs, upregulating the expression of DMP1, DSPP and BMP2, while downregulating ALP and RunX2. The differentiation induction by pDMP1- and pBMP2-NPs-hFDDSs was significantly higher than the positive control (dexamethasone). SEM revealed polarization of the differentiated cells, with processes extending into the natural dentinal tubules.
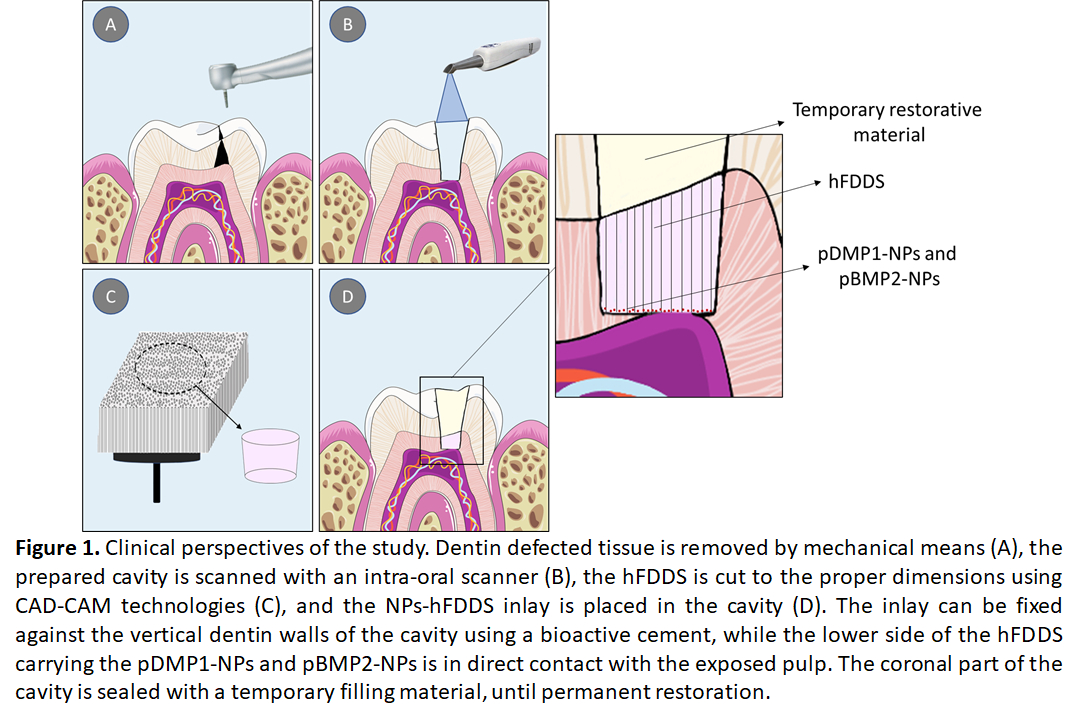
Conclusions: The proposed approach provides a promising bioactive dentin substitute and VPT tool that should be considered for clinical application in cases of deep lesions coming in direct/indirect contact with the pulp, promoting tissue healing and reparative dentin formation (Figure 1).
Methods: The hFDDSs were EDTA-treated, freeze-dried, and characterized by X-ray powder diffraction (XRD), confocal laser scanning microscopy (CLSM), and scanning electron microscopy (SEM). The CaP-NPs conjugated with plasmids encoding for Dentin Matrix Protein-1 (pDMP1) or Bone Morphogenetic Protein-2 (pBMP2) were synthesized, characterized, and tested in terms of biocompatibility (MTT assay), cellular uptake, and transfection efficiency [flow cytometry, transmission electron microscopy (TEM) and CLSM] on dental pulp stem cells (DPSCs). The construct of hFDDSs impregnated with NPs (NPs-hFDDSs) was tested for cytotoxicity (live/dead staining), and foreign body reaction in vivo (C57BL mice, N=4). Polarization of cells was evaluated by SEM, while odontogenic differentiation by qPCR.
Results: Based on the biocompatibility vs. transfectability results, nanoparticle concentration of 4-μg-Ca/mL was selected to prepare the NPs-hFDDSs. Biocompatibility of NPs-hFDDSs was similar to the control. In vivo experiments showed no foreign body reaction against the construct. DPSCs differentiated into polarized odontoblast-like cells on NPs-hFDDSs, upregulating the expression of DMP1, DSPP and BMP2, while downregulating ALP and RunX2. The differentiation induction by pDMP1- and pBMP2-NPs-hFDDSs was significantly higher than the positive control (dexamethasone). SEM revealed polarization of the differentiated cells, with processes extending into the natural dentinal tubules.
Conclusions: The proposed approach provides a promising bioactive dentin substitute and VPT tool that should be considered for clinical application in cases of deep lesions coming in direct/indirect contact with the pulp, promoting tissue healing and reparative dentin formation (Figure 1).