IADR Abstract Archives
3D Printing of Oral Muscle Tissues Based on Medical Imaging and Biological Hydrogels
Objectives: The surgical management of oral cavity cancers frequently involves the complete resection of the malignant lesion, along with a wide margin of surrounding tissues. This often results in significant functional compromise, given the critical role of oral musculature and mucosa in daily functions such as speech, mastication, and swallowing. The current standard of care involves reconstructions with autogenous tissue grafts, which necessitates the harvest of healthy tissues from the patient, alongside structural incompatibility between the harvested tissues and the recipient site. Unfortunately, this approach often fails to restore normal function while also causing tissue morbidity at the donor site.
The proposed project aims to create custom, patient-specific reconstructed oral soft tissues that mimic the resected site's anatomy and function, emphasizing muscle and epithelial architecture.
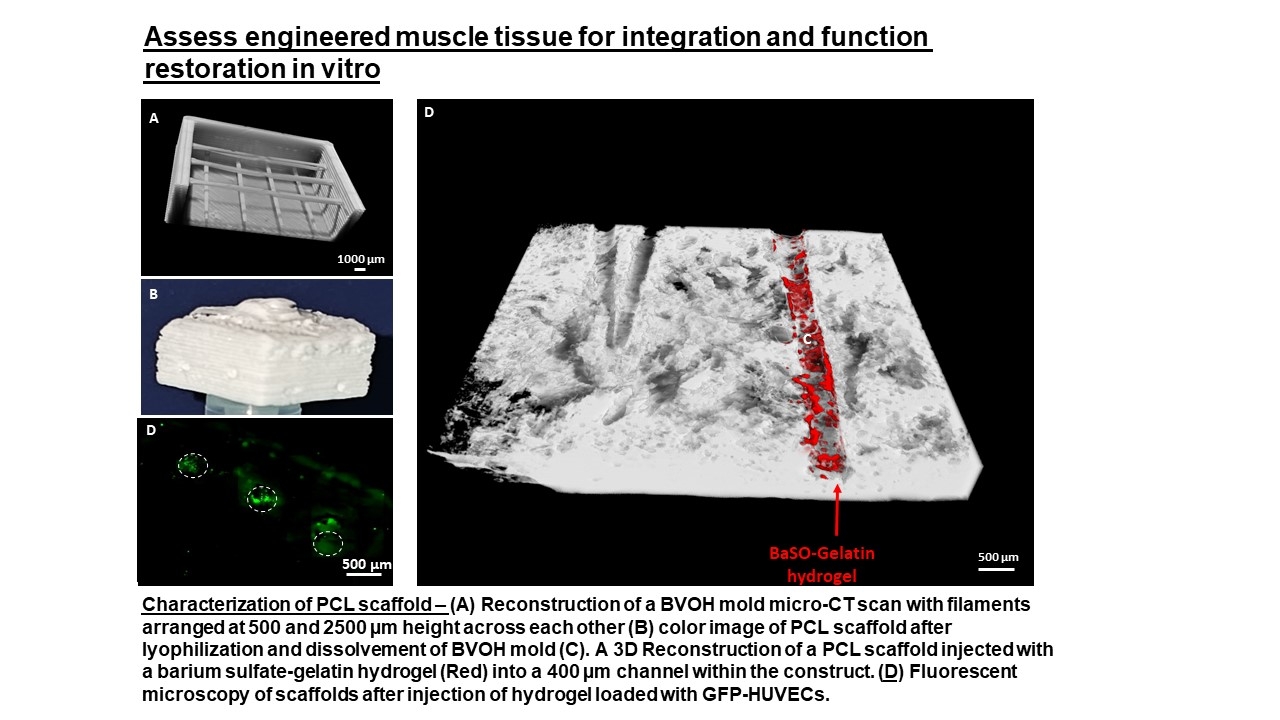
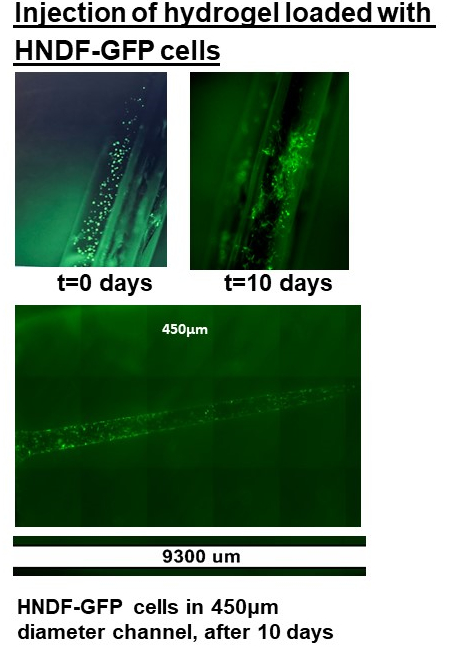
Methods: We achieve this by utilizing 3D printing of a sacrificial polymer to create an anatomically inspired scaffold derived from magnetic resonance imaging. The 3D-printed sacrificial polymeric mold is injected with polycaprolactone polymer, which, following a freeze-drying process in a high-power vacuum, will lead to the creation of the scaffold. The fabricated scaffolds are then loaded with collagen-based hydrogel to induce a favorable cellular loading and tissue maturation environment.
Results: Scaffolds were fabricated with appropriate microarchitecture to support tissue organization and tubular formation for muscle regeneration, which was evident from the micro-computed tomography of scaffolds before in vitro induction and in vivo implantation studies. In vivo, experiments indicated oral muscle tissue organization and mucosal coverage of scaffolds mimicking resected oral soft tissues, positive for both desmin and cytokeratin coupled with endothelial organization within implanted constructs. Finally, a large-scale sacrificial mold and polymeric construct were fabricated, affirming the possibility of creating a clinically-sized implant.
Conclusions: The following study provides a novel methodology for oral cancer rehabilitation with clear, clinically relevant implications.
The proposed project aims to create custom, patient-specific reconstructed oral soft tissues that mimic the resected site's anatomy and function, emphasizing muscle and epithelial architecture.
Methods: We achieve this by utilizing 3D printing of a sacrificial polymer to create an anatomically inspired scaffold derived from magnetic resonance imaging. The 3D-printed sacrificial polymeric mold is injected with polycaprolactone polymer, which, following a freeze-drying process in a high-power vacuum, will lead to the creation of the scaffold. The fabricated scaffolds are then loaded with collagen-based hydrogel to induce a favorable cellular loading and tissue maturation environment.
Results: Scaffolds were fabricated with appropriate microarchitecture to support tissue organization and tubular formation for muscle regeneration, which was evident from the micro-computed tomography of scaffolds before in vitro induction and in vivo implantation studies. In vivo, experiments indicated oral muscle tissue organization and mucosal coverage of scaffolds mimicking resected oral soft tissues, positive for both desmin and cytokeratin coupled with endothelial organization within implanted constructs. Finally, a large-scale sacrificial mold and polymeric construct were fabricated, affirming the possibility of creating a clinically-sized implant.
Conclusions: The following study provides a novel methodology for oral cancer rehabilitation with clear, clinically relevant implications.