IADR Abstract Archives
The Interplay of Mesenchymal Stem Cells and Neutrophils During Rapid Maxillary Expansion
Objectives: Objective: Rapid maxillary expansion (RME) is widely used by orthodontists in treating transverse deficient patients with various clinical responses. Although it is proposed that differences in calcification patterns of the suture, craniofacial architecture, and patient age are contributing factors, the biological basis underlying RME, the cell populations within mid-palatal suture, and cellular/molecular mechanisms in response to mechanical stimuli, are not well understood. Mesenchymal stem cells (MSCs) are a group of heterogeneous multipotent stem cells that can self-renew and further differentiate into several cell types, including osteoblasts, chondrocytes, and adipocytes, which have been explored extensively in regenerative medicine and bone remodeling. Osteoimmunology is an evolving concept promoting immune cells as emerging regulatory factors during bone remodeling via cross-talk between bone and the immune system. However, the role of the immune microenvironment in regulating MSCs, developmental growth, and RME is still under investigation. The goal of this study is to investigate the roles of MSCs and neutrophils residing in the mid-palatal suture and their interplay during maxillary expansion.
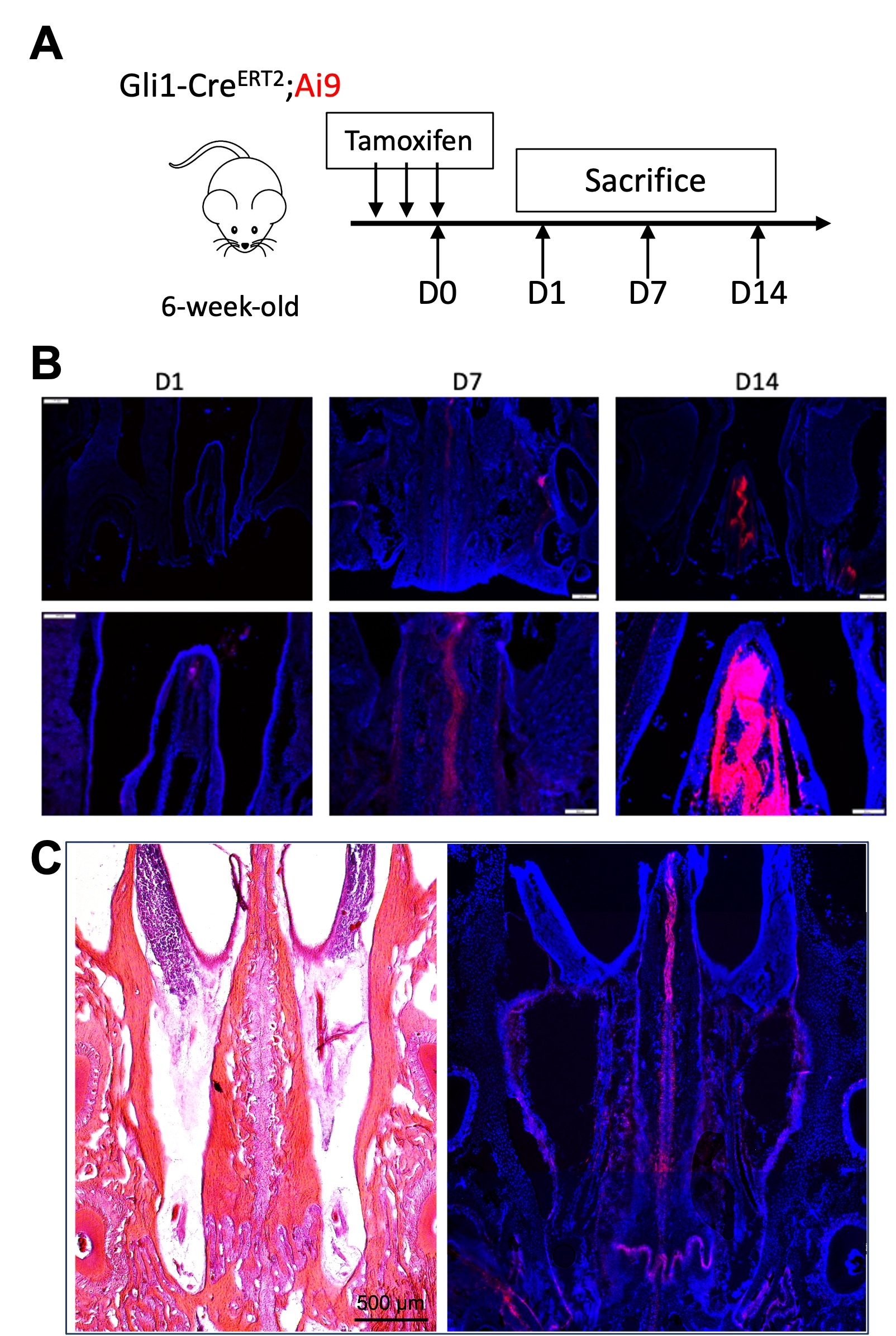
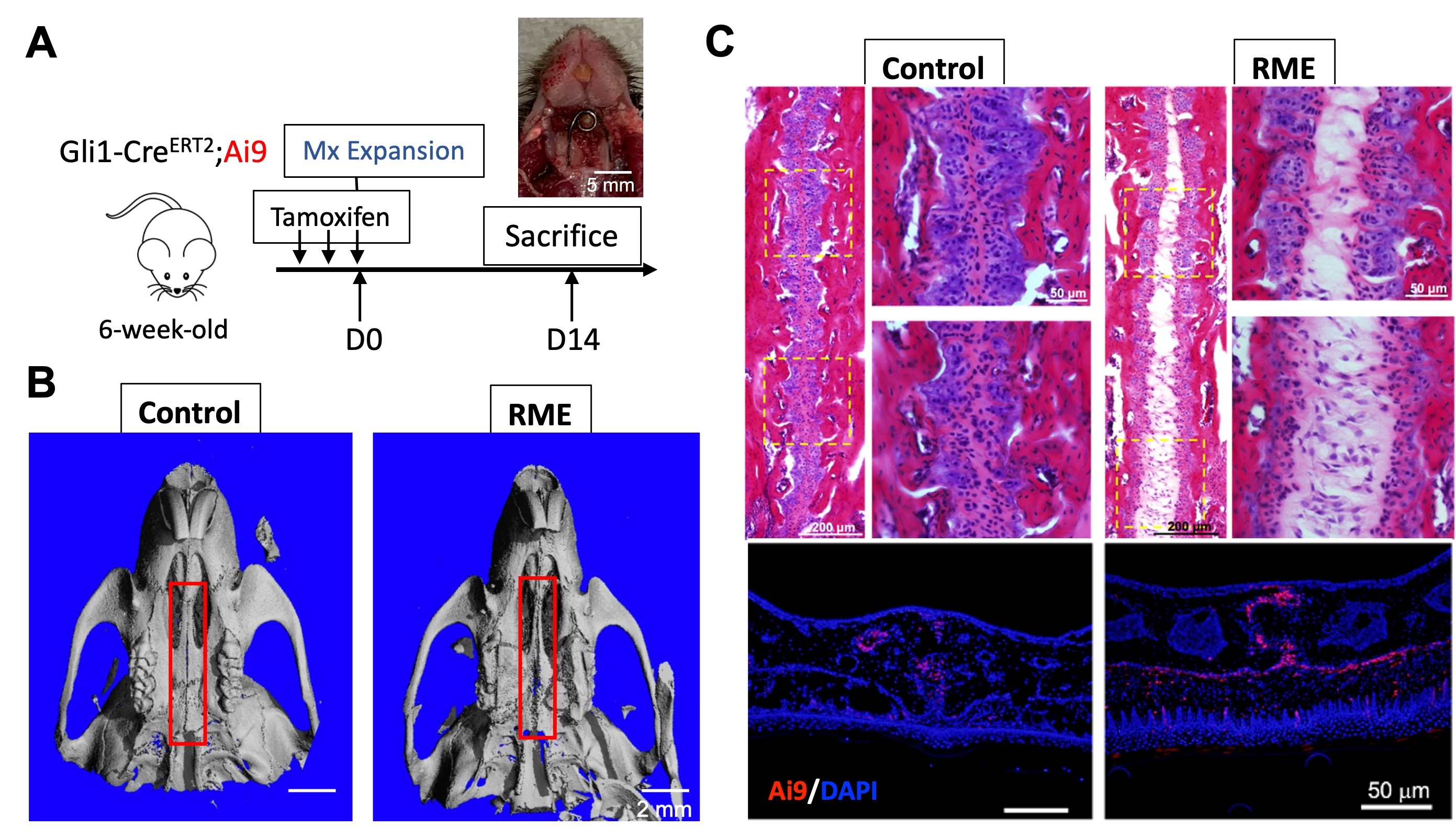
Methods: Maxillary mid-palatal expansion model was established using 6-8 weeks old Gli1-Cre;Ai9 mice. After 14-day expansion, maxilla tissue was harvested for micro-computed tomography (μCT) analysis, H&E staining, and immunofluorescent imaging. Cells isolated from mid-palatal suture were used for flow cytometry analysis, single-cell RNA sequencing, and MSC culture.
Results: 1. Gli1+ MSCs present within mid-palatal suture, which is critical to govern bone remodeling under maxillary expansion process.
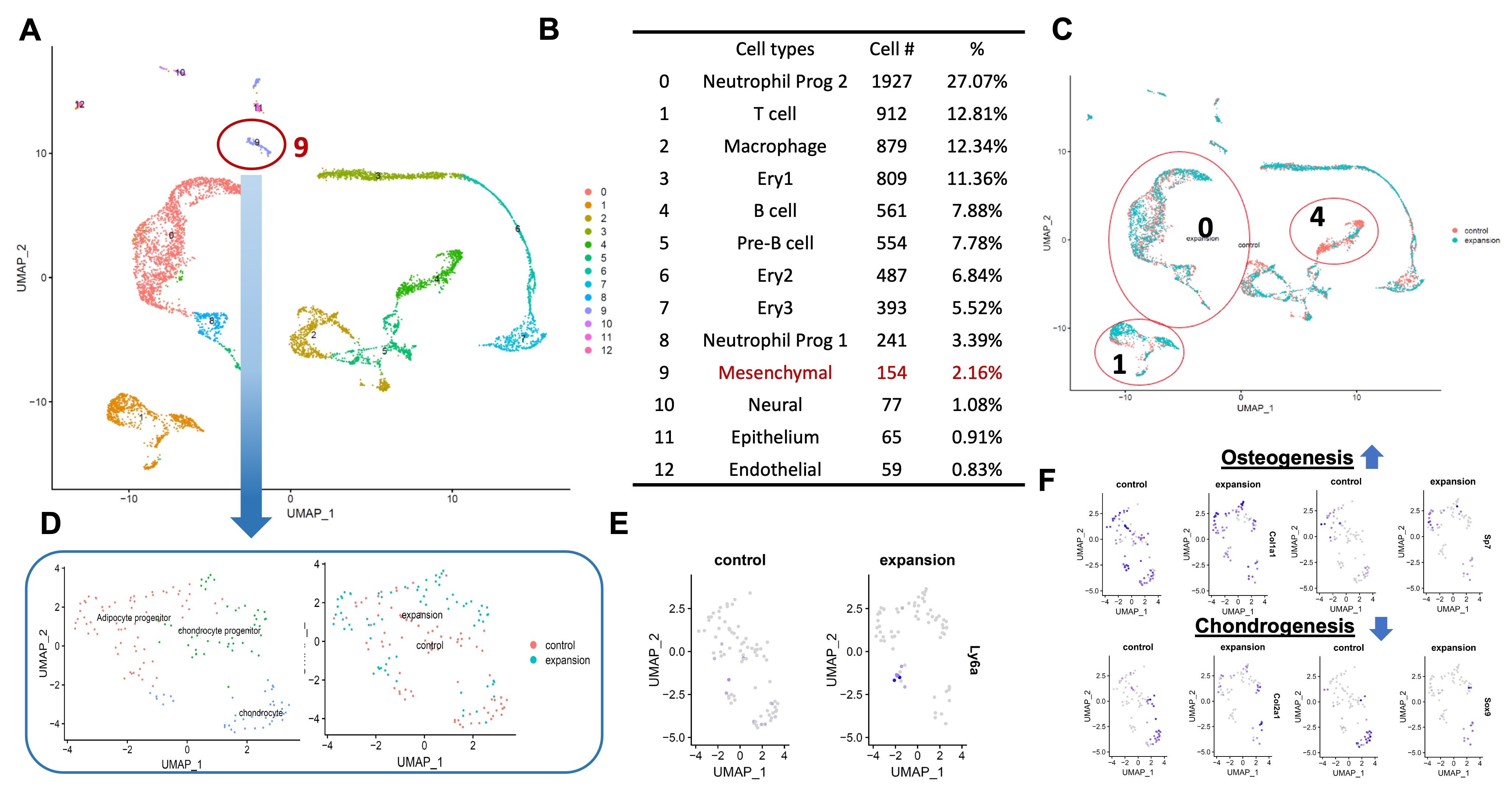
2. MSC lineage trajectories and the unique immune microenvironment have been revealed by single cell transcriptomics to depict the interplay between stem cells and surrounding immune microenvironment within mid-palatal suture.
3. An active immune microenvironment is identified in mid-palatal suture. The neutrophil, B cell and T cell subpopulations present most dramatic changes in response to RPE.
Conclusions: This study reveals novel mechanisms that affect RME efficacy, providing a new paradigm to delineate immune-MSC modulatory machinery during expansion precisely.
Methods: Maxillary mid-palatal expansion model was established using 6-8 weeks old Gli1-Cre;Ai9 mice. After 14-day expansion, maxilla tissue was harvested for micro-computed tomography (μCT) analysis, H&E staining, and immunofluorescent imaging. Cells isolated from mid-palatal suture were used for flow cytometry analysis, single-cell RNA sequencing, and MSC culture.
Results: 1. Gli1+ MSCs present within mid-palatal suture, which is critical to govern bone remodeling under maxillary expansion process.
2. MSC lineage trajectories and the unique immune microenvironment have been revealed by single cell transcriptomics to depict the interplay between stem cells and surrounding immune microenvironment within mid-palatal suture.
3. An active immune microenvironment is identified in mid-palatal suture. The neutrophil, B cell and T cell subpopulations present most dramatic changes in response to RPE.
Conclusions: This study reveals novel mechanisms that affect RME efficacy, providing a new paradigm to delineate immune-MSC modulatory machinery during expansion precisely.