IADR Abstract Archives
Elucidating the Effects of Botox on TMD and PTSD Symptoms
Objectives: Temporomandibular Joint Disorder (TMD) is a poorly understood disease that affects 10-25% of the population. Among the veteran population, it often co-presents with Post Traumatic Stress Disorder (PTSD). We discovered Botox decreases TMD-related pain and reduces the symptoms of PTSD, particularly the anxiety and hypervigilance states. Further, the actions and time-course of Botox on the muscles is surprisingly ill-defined in relation to pain reduction. Our study aims are two-fold: one is to to precisely define the actions of Botox on muscle volume and strength, change in pain scores, and PTSD symptoms; and second is to use the pain-relieving aspect of Botox as a tool to better understand the connection between chronic pain and PTSD.
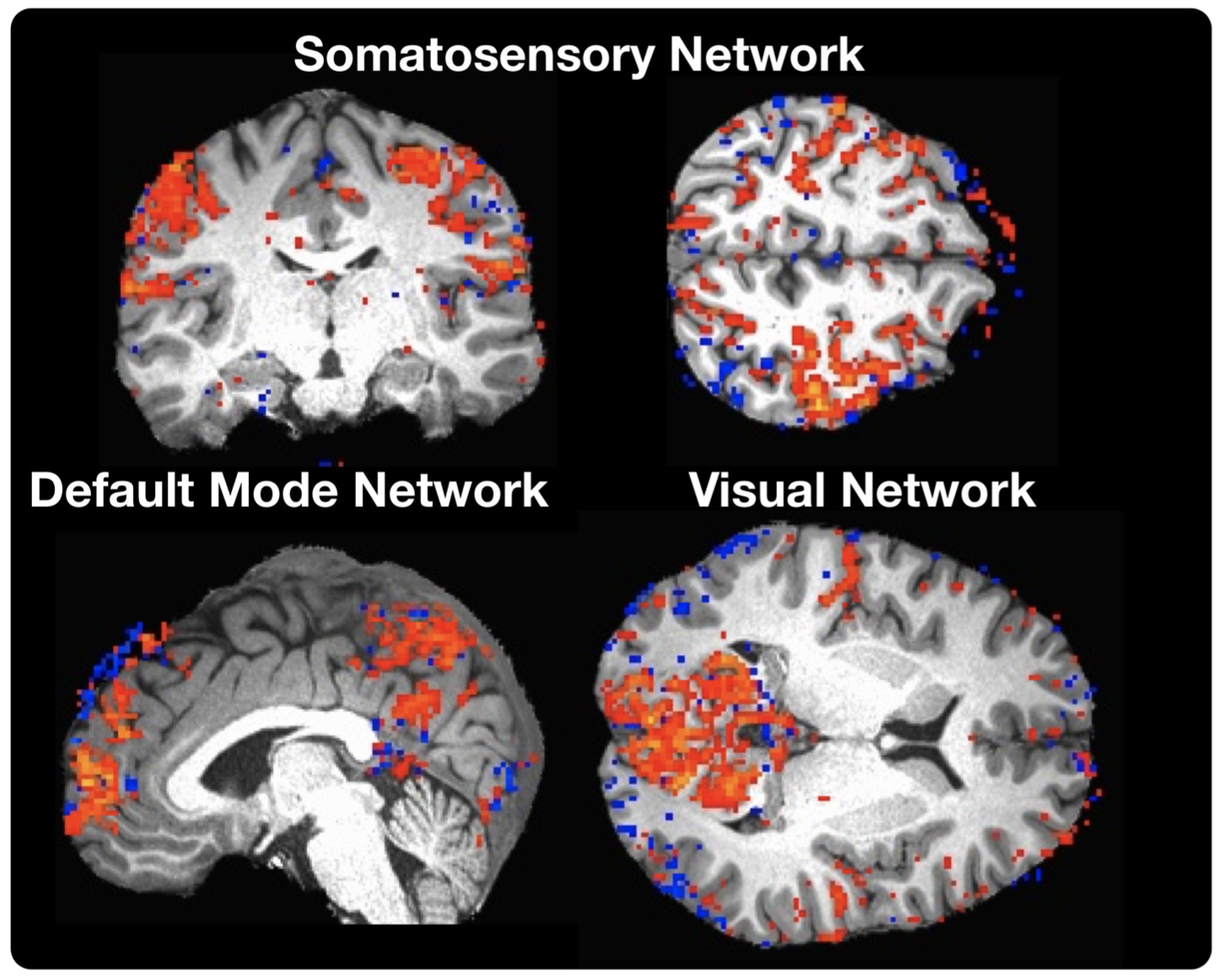
Methods: In this pilot study, two patients met the requirements for a diagnosis of TMD and PTSD. They completed questionnaires to evaluate pain and PTSD symptoms, enrolled in a daily pain application, had Electromyelography (EMG) to evaluate muscle function, and an ultrasound of the Masseter, Temporalis, and Sternocleidomastoid (SCM) muscles to measure muscle thickness before Botox injections. Lastly, they underwent a resting state evaluation and imaging of the trigeminal nucleus via fMRI. After preliminary testing was done, patients received onabotulinum toxin (Botox) injections (100 units/4cc saline) into the Masseter and Temporalis.
Results: Two patients have completed phase one of the study. Data compared before and after injections showed a decrease in average daily pain from a 6 and 9 respectively, to a 2.4 and a 1.1 on the visual analog scale. One patient showed a marked decrease in the incidence of nightmares associated with PTSD.
Conclusions: In phase 2 of this pilot study, we expect to see an alteration in the connectivity of regions of the brain involved in PTSD and TMD after post-injection imaging, a reduction in the pain severity questionnaires, and a decrease in muscle thickness of the masseter and temporalis with no change in the SCM. Clinically, patients should experience less pain from TMJ, and should see a reduction in PTSD symptoms.
Methods: In this pilot study, two patients met the requirements for a diagnosis of TMD and PTSD. They completed questionnaires to evaluate pain and PTSD symptoms, enrolled in a daily pain application, had Electromyelography (EMG) to evaluate muscle function, and an ultrasound of the Masseter, Temporalis, and Sternocleidomastoid (SCM) muscles to measure muscle thickness before Botox injections. Lastly, they underwent a resting state evaluation and imaging of the trigeminal nucleus via fMRI. After preliminary testing was done, patients received onabotulinum toxin (Botox) injections (100 units/4cc saline) into the Masseter and Temporalis.
Results: Two patients have completed phase one of the study. Data compared before and after injections showed a decrease in average daily pain from a 6 and 9 respectively, to a 2.4 and a 1.1 on the visual analog scale. One patient showed a marked decrease in the incidence of nightmares associated with PTSD.
Conclusions: In phase 2 of this pilot study, we expect to see an alteration in the connectivity of regions of the brain involved in PTSD and TMD after post-injection imaging, a reduction in the pain severity questionnaires, and a decrease in muscle thickness of the masseter and temporalis with no change in the SCM. Clinically, patients should experience less pain from TMJ, and should see a reduction in PTSD symptoms.