IADR Abstract Archives
Adaptive Biomechanics of Diseased Dentoalveolar Joints
Objectives: Disease-induced changes in biomechanics can prompt tissue adaptation farther from the inflammation site. In this study, changes in biomechanics of diseased alveolar bone (AB)-periodontal ligament (PDL)-tooth fibrous joints was correlated with changes in mineral formation rates at the PDL-bone and PDL-cementum interfaces of the joints.
Methods: In situ biomechanical testing coupled with micro X-ray computed tomography (µ-XCT) was performed on ligated (6, 12-week) and control groups. The relative movement between tooth and AB under load(5, 10, 15N) was calculated by digitally correlating µ-XCT tomograms at unloaded to loaded conditions. Morphometrics related to mineral formation at biomechanically active sites, such as interradicular bone, alveolar crest, apical cementum were also investigated using fluorochrome treated rats.
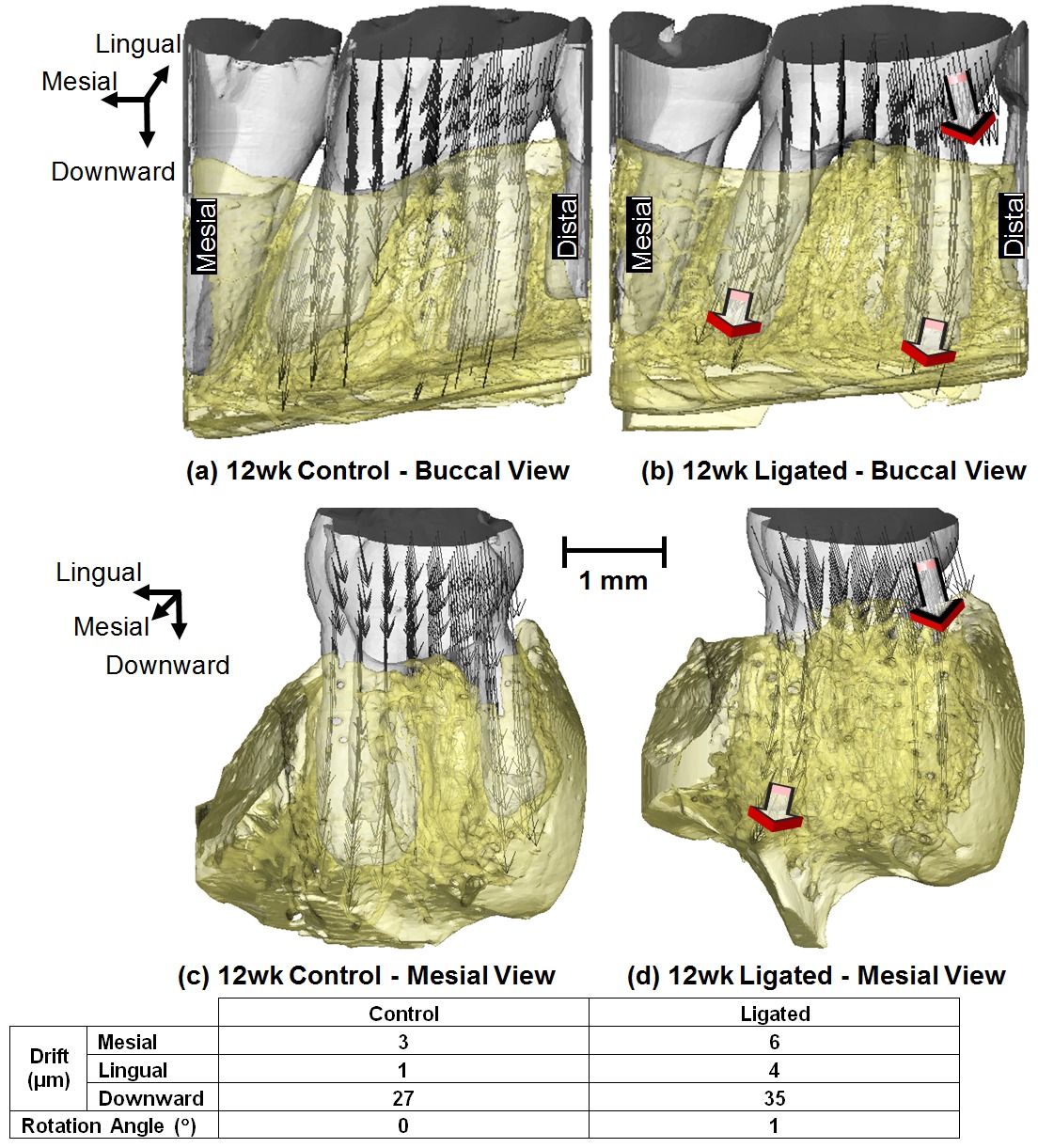
Results: At 6 and 12 weeks, diseased joints exhibited lower stiffness (639-683, 608-670N/mm) compared to controls (681-735, 691-753N/mm). An increased tooth movement inside the alveolar socket was observed in 12wk ligated molars in all directions. Increased lateral movement of ligated teeth (Fig.1) was correlated to significant resorption at interproximal and interradicular AB of diseased complexes. Increased pitting was observed at the distal root surfaces of ligated molars, along with widening of the PDL-space (20-45µm). Moreover, with the onset of periodontitis, fluorochrome markers showed that the AB apposition rate was increased by 48%, 15% and 27% in the interradicular, interproximal and crestal regions, respectively.
Conclusions: Results show that ligated teeth have increased movement in the alveolar socket, and that bone apposition rate increased at the interradicular, interproximal and crestal regions. We propose that the increased degrees of freedom of tooth under functional loads can stimulate bone metabolism, especially at biomechanically active sites. However, tissue adaptations, resulting from disease-altered mechanobiological effects, can impair overall joint function. From a clinical perspective, results of this study provide insights to reversible adaptations through load modulation to regain optimum function.
Methods: In situ biomechanical testing coupled with micro X-ray computed tomography (µ-XCT) was performed on ligated (6, 12-week) and control groups. The relative movement between tooth and AB under load(5, 10, 15N) was calculated by digitally correlating µ-XCT tomograms at unloaded to loaded conditions. Morphometrics related to mineral formation at biomechanically active sites, such as interradicular bone, alveolar crest, apical cementum were also investigated using fluorochrome treated rats.
Results: At 6 and 12 weeks, diseased joints exhibited lower stiffness (639-683, 608-670N/mm) compared to controls (681-735, 691-753N/mm). An increased tooth movement inside the alveolar socket was observed in 12wk ligated molars in all directions. Increased lateral movement of ligated teeth (Fig.1) was correlated to significant resorption at interproximal and interradicular AB of diseased complexes. Increased pitting was observed at the distal root surfaces of ligated molars, along with widening of the PDL-space (20-45µm). Moreover, with the onset of periodontitis, fluorochrome markers showed that the AB apposition rate was increased by 48%, 15% and 27% in the interradicular, interproximal and crestal regions, respectively.
Conclusions: Results show that ligated teeth have increased movement in the alveolar socket, and that bone apposition rate increased at the interradicular, interproximal and crestal regions. We propose that the increased degrees of freedom of tooth under functional loads can stimulate bone metabolism, especially at biomechanically active sites. However, tissue adaptations, resulting from disease-altered mechanobiological effects, can impair overall joint function. From a clinical perspective, results of this study provide insights to reversible adaptations through load modulation to regain optimum function.